Analysis of Psoriasis: Understanding Immune System Dysregulation and Management Strategies
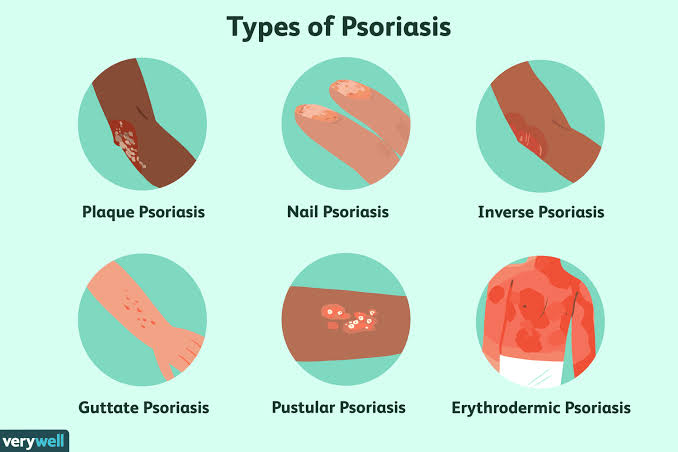
Psoriasis is a chronic skin condition characterized by immune system dysfunction, leading to the accumulation of inflammatory cells in the dermis and accelerated growth of skin cells in the epidermis. This immune-mediated process results in uncomfortable symptoms, including raised plaques, scales, swelling, and redness or discoloration. Understanding the underlying mechanisms of psoriasis is crucial for effective management and improved quality of life for individuals affected by this condition.
Immune System Dysfunction: In psoriasis, immune system dysregulation triggers an inflammatory response, causing an abnormal buildup of inflammatory cells in the dermis. Simultaneously, the growth of skin cells in the epidermis accelerates, leading to a rapid turnover of cells. While normal skin cell turnover takes about a month, individuals with psoriasis experience this process in just a few days. The accumulation of skin cells on the surface contributes to the characteristic symptoms of psoriasis.
Systemic Impact: While psoriasis primarily manifests as a skin condition, the inflammation associated with it has systemic implications. Research indicates an increased risk of various health conditions, including heart disease, cancer, inflammatory bowel disease, and psoriatic arthritis. This highlights the importance of viewing psoriasis as a condition that goes beyond the skin, emphasizing the need for comprehensive healthcare management.
Management Approaches: Studies suggest that lifestyle and dietary changes can play a role in reducing inflammation associated with psoriasis. These changes may help alleviate symptoms and enhance overall well-being. Additionally, various medications are available to manage psoriasis, targeting the underlying inflammatory processes. Topical corticosteroids, injectable biologics, and oral medications are among the options that healthcare professionals may prescribe based on the severity of symptoms and individual response.
Individualized Treatment: It’s essential to recognize the individual variability in psoriasis manifestations. Each person may require a unique approach to treatment, considering factors such as symptom severity, response to medications, and overall health. Achieving and maintaining remission, characterized by a prolonged period without psoriasis symptoms, is a goal that can be pursued through tailored treatment plans.
Collaborative Healthcare Approach: Individuals experiencing psoriasis flares are encouraged to consult their healthcare team, including dermatologists, for personalized guidance. Healthcare professionals can assess symptom severity, recommend suitable treatment methods, and provide insights into lifestyle and dietary modifications. A collaborative approach ensures that individuals with psoriasis receive comprehensive care addressing both skin-related symptoms and potential systemic implications.
In summary, understanding the complex interplay of immune system dysfunction in psoriasis allows for targeted management strategies. Through a combination of lifestyle changes, medications, and individualized treatment plans, individuals with psoriasis can work towards reducing inflammation, managing symptoms, and improving their overall quality of life. Regular communication with healthcare professionals remains integral to achieving optimal outcomes in psoriasis management.


