Recent Study Identifies Genetic Factors Modifying the Impact of Diet on Colorectal Cancer Risk
In a recent study published in the journal eBioMedicine, researchers conducted a comprehensive genome-wide interaction analysis to explore how genetic variants may alter the relationship between dietary intake and colorectal cancer (CRC) risk. This study successfully identified two significant loci that modify the association of fiber and fruit intake with CRC risk.
Background and Significance
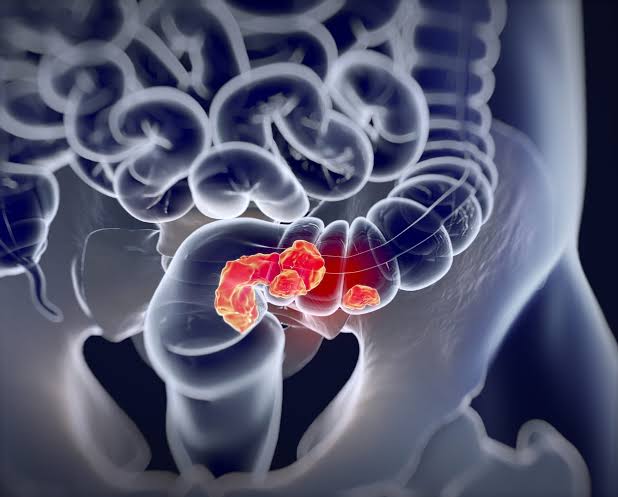
Colorectal cancer remains a major global health concern, with nearly two million new cases and over 900,000 deaths reported in 2020. Epidemiological evidence suggests that a diet high in fruits, vegetables, whole grains, and dietary fiber can reduce the risk of CRC. However, while the protective effects of whole grains and fiber are well-documented, the evidence for fruits and vegetables remains less definitive.
Previous genome-wide association studies (GWAS) have identified over 200 loci linked to CRC risk, accounting for up to 35% of its heritability. Gene-environment interactions (G × E) may explain additional heritability, but prior studies, often limited by small sample sizes and traditional methods, have found few significant gene-diet interactions. This study aimed to overcome these limitations using advanced statistical approaches and a large dataset.
Study Design and Methods
The analysis included data from up to 45 studies from three CRC genetic consortia, involving individuals of European ancestry. The dataset comprised 69,599, 69,734, and 44,890 participants for analyses of fruit, vegetable, and fiber intake, respectively. Dietary intake was measured using food frequency questionnaires and diet histories, typically quantified as servings per day for fruits and vegetables, and grams per day for total fiber.
Genotyping quality control involved stringent screening and filtering, resulting in 7,250,911 single nucleotide polymorphisms (SNPs) for analysis. Genome-wide interaction scans employed both traditional logistic regression models and advanced techniques like the 3-DF joint test and the two-step approach. Additionally, interaction analyses for rare variants were conducted using the MiSTi method.
Key Findings
Compared to controls, CRC patients were generally older, had higher body mass indices, and a greater prevalence of risk factors such as family history of CRC and type 2 diabetes. They also consumed less fiber, fruits, and vegetables. Meta-analyses revealed inverse associations between fiber (odds ratio per quartile increase (OR) = 0.79), fruit (OR = 0.79), and vegetable (OR = 0.82) intake and CRC risk, with stronger effects observed in case-control studies.
The 3-DF joint test identified the rs4730274 locus upstream of the SLC26A3 gene, associated with fiber intake and interaction with CRC risk. Stratification by genotype indicated a stronger inverse association between fiber intake and CRC for each T allele copy. Functional annotations suggested enhancer activity in colon tissues, with expression quantitative trait loci (eQTLs) for the DLD gene supporting these findings.
Additionally, the rs1620977 locus near the NEGR1 gene showed a significant association with fruit intake and a modest interaction with CRC risk. A stronger inverse association was observed with increased fruit intake for each G allele copy. No significant interaction effects were identified for vegetable intake.
Strengths and Limitations
The study’s strengths include its large sample size, advanced statistical methods, and rigorous data quality control. However, limitations include reliance on single questionnaire measurements for dietary intake, inability to analyze different types of fiber, potential biases inherent in case-control studies, and generalizability limited to populations of European ancestry.
Conclusion
This study represents the most extensive G × E analysis of its kind, identifying significant interactions between dietary fiber and fruit intake and CRC risk. Specifically, the rs4730274 locus near the SLC26A3 gene underscores the link between fiber consumption, gut function, inflammation, and CRC risk. These findings highlight the need for further research to explore the clinical implications and validate these results across diverse populations.


